Proactive Diagnostics: Why We Must Screen the Heart and Kidneys Simultaneously.
Cardiovascular disease (CVD) and chronic kidney disease (CKD) are two of the most prevalent and costly health conditions worldwide. Traditionally viewed as distinct clinical entities, contemporary research — including recent evidence published in the Journal of the American Heart Association (JAHA) — has reinforced that CVD and CKD are deeply interconnected through shared pathophysiological mechanisms. This convergence not only explains their frequent coexistence but also highlights the urgent need for early screening and integrated management strategies.
Shared Pathogenesis: A Common Disease Continuum
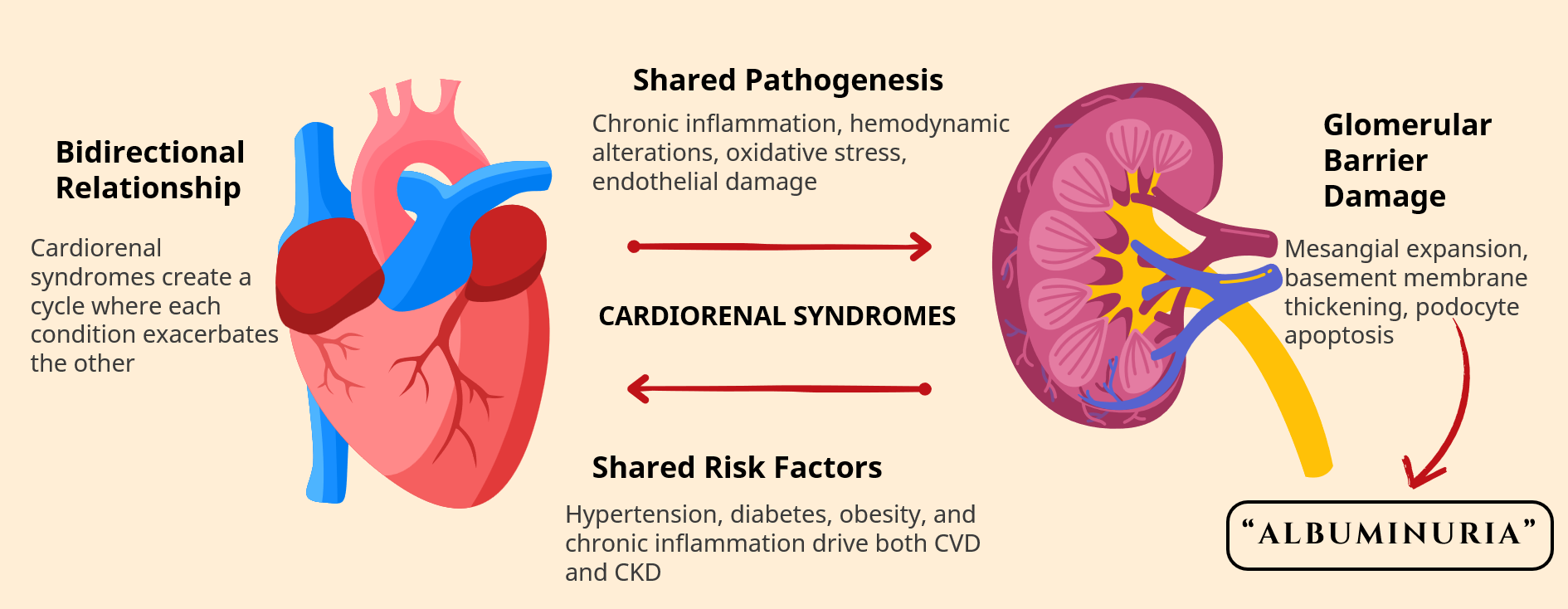
CVD and CKD are being increasingly recognized as manifestations of a single systemic vascular disorder. Both conditions are driven by overlapping mechanisms, including endothelial dysfunction, chronic inflammation, oxidative stress, activation of the renin–angiotensin–aldosterone system (RAAS), and metabolic dysregulation. These processes promote progressive vascular damage, microvascular rarefaction, and impaired organ perfusion — ultimately affecting both the heart and the kidneys.
The JAHA publication underscores that kidney dysfunction is not merely a consequence of cardiovascular pathology, nor is cardiovascular disease solely a complication of renal impairment. Instead, they evolve together through a bidirectional and self-amplifying disease process, often referred to as the cardio-renal continuum. This shared pathogenesis explains why patients with early kidney damage face a substantially elevated risk of myocardial infarction, heart failure, arrhythmias, and premature mortality, even before overt declines in glomerular filtration rate (GFR) are observed.
Albuminuria: A Critical Link Between CKD and CVD
Albuminuria is defined as the abnormal leakage of albumin into the urine. It has emerged as one of the most powerful and independent predictors of both kidney disease progression and cardiovascular morbidity and mortality. Albuminuria reflects systemic endothelial dysfunction and increased vascular permeability, rather than being solely a marker of renal injury.
Clinically, even low-grade elevations in urinary albumin excretion (microalbuminuria) are associated with significantly increased risks of coronary artery disease, stroke, heart failure, and all-cause mortality — independent of estimated GFR (eGFR). Similarly, in patients without overt CKD, albuminuria identifies a high-risk phenotype for future renal decline and cardiovascular events.
Importantly, albuminuria serves as a shared biomarker of microvascular damage across multiple organ systems. Its presence indicates not only glomerular injury but also widespread vascular pathology affecting the myocardium, cerebral circulation, and peripheral vasculature. This makes albuminuria a pivotal diagnostic and prognostic tool in both nephrology and cardiology.
The Imperative for Early Screening and Integrated Management
Given the intertwined nature of CVD and CKD, early detection of albuminuria and kidney dysfunction is essential for effective risk stratification and disease modification. Reliance on serum creatinine or eGFR alone may miss early renal injury and underestimate cardiovascular risk. Incorporating routine screening for urinary albumin-to-creatinine ratio (uACR) enables clinicians to identify high-risk individuals at an earlier, more reversible stage of disease.
Early intervention in patients with albuminuria has been shown to reduce both renal and cardiovascular outcomes through evidence-based therapies such as RAAS inhibitors, sodium-glucose cotransporter-2 (SGLT2) inhibitors, blood pressure optimization, glycemic control, lipid management, and lifestyle modification. These interventions act on the shared disease pathways, thereby attenuating progression across both organ systems.
From a public health perspective, integrating kidney and cardiovascular risk screening into primary care — particularly for individuals with diabetes, hypertension, obesity, or a family history of vascular disease — represents a high-yield strategy for reducing long-term morbidity, mortality, and healthcare costs.
Conclusion
The emerging body of evidence, including the referenced JAHA publication, clearly establishes that CVD and CKD are not isolated diseases but rather interconnected manifestations of systemic vascular pathology. Albuminuria stands at the center of this relationship, serving as both an early marker of kidney injury and a powerful predictor of cardiovascular risk. Recognizing this shared pathogenesis underscores the critical importance of early screening, proactive risk stratification, and integrated cardio-renal management. By identifying and addressing disease at its earliest stages, clinicians can significantly improve patient outcomes and alter the trajectory of two of the most burdensome chronic diseases globally.
Reference: Albuminuria: An Underappreciated Risk Factor for Cardiovascular Disease
Joshua I Barzilay, MD; Youssef M. K. Farag, MD, PhD; Jeffrey Durthaler
https://doi.org/10.1161/JAHA.123.030131

